Performance Evaluation of Low-Cost Airborne Infection Isolation Room
doi: 10.14456/mijet.2024.1
Keywords:
Performance, low-cost controller, airborne infection isolation room, Covid-19Abstract
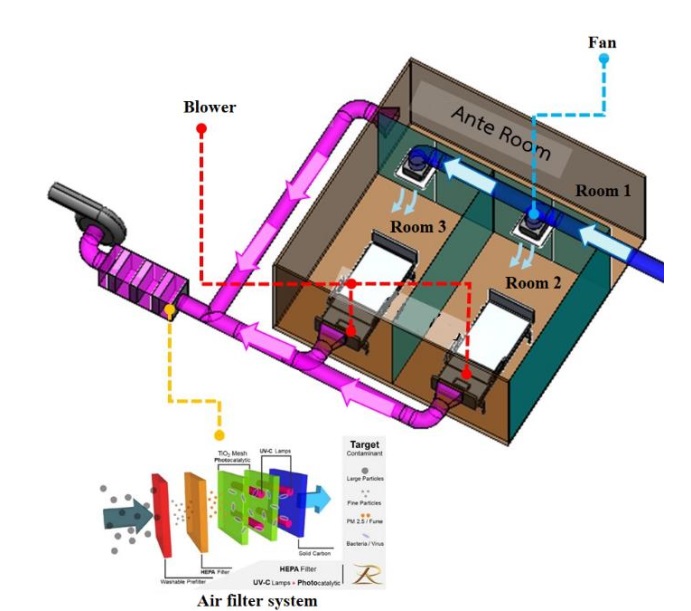
This study presents the performance of a low-cost airborne infection isolation room (AIIR). The system consists of an ante room, two AIIRs, a blower, two butterfly valves, an air conditioner, a controller, and a ventilation system. Pressure and temperature sensors were calibrated and installed in all rooms. The control was an in-house system, including Arduino Uno R3, ESP32, NI-USB 6009, and PLC FX5U. PID control was employed to regulate the pressure inside the AIIRs by adjusting the outlet air blower speed. The system was tested under various negative pressures, i.e. -2.5 to -10 Pa, and the effect of inlet opening was also investigated. The results showed that the system effectively controlled the pressure under all experimental conditions. The blower speed and room pressure were found to be related, with higher blower speeds required when all butterfly valves were open. The current of the motor increased with the valve set connected, and the highest current was observed when all butterfly valves were open. The air velocity generated by the blower suction varied with the room pressure, with a decrease in pressure leading to an increase in air velocity. However, for one room operation, the velocity difference was insignificant.
References
T. T. Chow and X. Y. Yang, “Ventilation performance in the operating theatre against airborne infection: numerical study on an ultra-clean system,” J. Hosp. Infect., vol. 59, no. 2, pp. 138–147, Feb. 2005, doi: 10.1016/j.jhin.2004.09.006.
H. Y. Kek et al., “Ventilation strategies for mitigating airborne infection in healthcare facilities: A review and bibliometric analysis (1993–2022),” Energy Build., vol. 295, p. 113323, Sep. 2023, doi: 10.1016/j.enbuild.2023.113323.
Y. Zhou, Y. Zeng, and C. Chen, “Presence of SARS-CoV-2 RNA in isolation ward environment 28 days after exposure,” Int. J. Infect. Dis., vol. 97, pp. 258–259, Aug. 2020, doi: 10.1016/j.ijid.2020.06.015.
Z. Liu, R. Li, Y. Wu, R. Ju, and N. Gao, “Numerical study on the effect of diner divider on the airborne transmission of diseases in canteens,” Energy Build., vol. 248, p. 111171, Oct. 2021, doi: 10.1016/j.enbuild.2021.111171.
Y. Bi, A. Aganovic, H. M. Mathisen, and G. Cao, “Experimental study on the exposure level of surgical staff to SARS-CoV-2 in operating rooms with mixing ventilation under negative pressure,” Build. Environ., vol. 217, p. 109091, Jun. 2022, doi: 10.1016/j.buildenv.2022.109091.
B. C. H. Tsui and S. Pan, “Are aerosol-generating procedures safer in an airborne infection isolation room or operating room?,” Br. J. Anaesth., vol. 125, no. 6, pp. e485–e487, Dec. 2020, doi: 10.1016/j.bja.2020.09.011.
J. Wang and T.-T. Chow, “Numerical investigation of influence of human walking on dispersion and deposition of expiratory droplets in airborne infection isolation room,” Build. Environ., vol. 46, no. 10, pp. 1993–2002, Oct. 2011, doi: 10.1016/j.buildenv.2011.04.008.
B. Blocken et al., “Ventilation and air cleaning to limit aerosol particle concentrations in a gym during the COVID-19 pandemic,” Build. Environ., vol. 193, p. 107659, Apr. 2021, doi: 10.1016/j.buildenv.2021.107659.
F. A. Berlanga, M. R. de Adana, I. Olmedo, J. M. Villafruela, J. F. San José, and F. Castro, “Experimental evaluation of thermal comfort, ventilation performance indices and exposure to airborne contaminant in an airborne infection isolation room equipped with a displacement air distribution system,” Energy Build., vol. 158, pp. 209–221, Jan. 2018, doi: 10.1016/j.enbuild.2017.09.100.
G. Pei, M. Taylor, and D. Rim, “Human exposure to respiratory aerosols in a ventilated room: Effects of ventilation condition, emission mode, and social distancing,” Sustain. Cities Soc., vol. 73, p. 103090, Oct. 2021, doi: 10.1016/j.scs.2021.103090.
H. Liu et al., “Reducing airborne transmission of SARS-CoV-2 by an upper-room ultraviolet germicidal irradiation system in a hospital isolation environment,” Environ. Res., vol. 237, p. 116952, Nov. 2023, doi: 10.1016/j.envres.2023.116952.
A. Giffin, W. Gong, S. Majumder, A. G. Rappold, B. J. Reich, and S. Yang, “Estimating intervention effects on infectious disease control: The effect of community mobility reduction on Coronavirus spread,” Spat. Stat., vol. 52, p. 100711, Dec. 2022, doi: 10.1016/j.spasta.2022.100711.
J. Lin et al., “Containing the spread of coronavirus disease 2019 (COVID-19): Meteorological factors and control strategies,” Sci. Total Environ., vol. 744, p. 140935, Nov. 2020, doi: 10.1016/j.scitotenv.2020.140935.
L. Lu, Q. Liu, L. Du, and S. Jiang, “Middle East respiratory syndrome coronavirus (MERS-CoV): challenges in identifying its source and controlling its spread,” Microbes Infect., vol. 15, no. 8, pp. 625–629, Jul. 2013, doi: 10.1016/j.micinf.2013.06.003.
G. N. Nurkahfi et al., “Development of a low-cost wearable device for Covid-19 self-quarantine monitoring system,” Public Health Pract., vol. 4, p. 100299, Dec. 2022, doi: 10.1016/j.puhip.2022.100299.
A. Kouidere, L. E. Youssoufi, H. Ferjouchia, O. Balatif, and M. Rachik, “Optimal Control of Mathematical modeling of the spread of the COVID-19 pandemic with highlighting the negative impact of quarantine on diabetics people with Cost-effectiveness,” Chaos Solitons Fractals, vol. 145, p. 110777, Apr. 2021, doi: 10.1016/j.chaos.2021.110777.
L. Y. Y. Lee et al., “Quantifying the reduction of airborne infectious viral load using a ventilated patient hood,” J. Hosp. Infect., vol. 136, pp. 110–117, Jun. 2023, doi: 10.1016/j.jhin.2023.04.009.
V. Bergeron et al., “Supplemental treatment of air in airborne infection isolation rooms using high-throughput in-room air decontamination units,” Am. J. Infect. Control, vol. 39, no. 4, pp. 314–320, May 2011, doi: 10.1016/j.ajic.2010.06.013.
R. Sukarno, N. Putra, I. I. Hakim, F. F. Rachman, and T. M. Indra Mahlia, “Utilizing heat pipe heat exchanger to reduce the energy consumption of airborne infection isolation hospital room HVAC system,” J. Build. Eng., vol. 35, p. 102116, Mar. 2021, doi: 10.1016/j.jobe.2020.102116.
N. Nuntapap et al., “Airborne Infection Isolation Room with Low-Cost Operating System,” Eng. Access, vol. 9, no. 1, Art. no. 1, 2023.
N. Deb, S. Fardin, M. M. Fardin, N. Nawal, M. R. Nizam, and S. Saha, “Thermal management inside a discretely heated rectangular cuboid using P, PI and PID controllers,” Case Stud. Therm. Eng., vol. 51, p. 103601, Nov. 2023, doi: 10.1016/j.csite.2023.103601.
S. Sangeetha, B. S. Revathi, K. Balamurugan, and S. G., “Performance analysis of buck converter with fractional PID controller using hybrid technique,” Robot. Auton. Syst., vol. 169, p. 104515, Nov. 2023, doi: 10.1016/j.robot.2023.104515.
Y. Ye, Y. Wang, L. Wang, and X. Wang, “A modified predictive PID controller for dynamic positioning of vessels with autoregressive model,” Ocean Eng., vol. 284, p. 115176, Sep. 2023, doi: 10.1016/j.oceaneng.2023.115176.
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.








