Effective behavioral interventions for smoking cessation in the primary care setting: A meta-analysis.
Main Article Content
Abstract
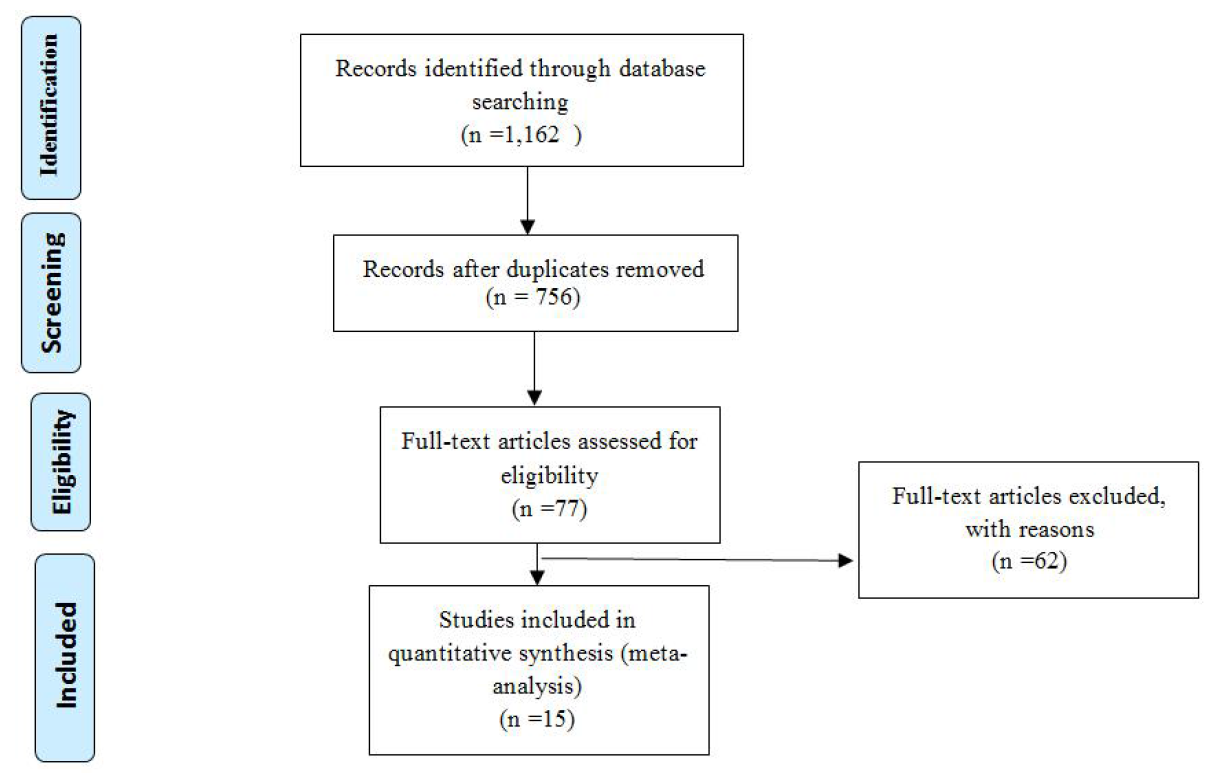
There are a number of smoking cessation strategies offered by healthcare providers in Thailand. Despite this, the number of Thai smokers have stopped smoking permanently as a result of the strategies is still far less than the expectation of the National Strategic Plan for Tobacco Control. It feels that this is a reflection of the fact that there are a lot of delicate issues around use of the tobacco cessation service system. This research aimed to investigate the effectiveness of strategies for smoking cessation intervention among smokers in the primary care setting on point prevalence abstinence (PPA) basis. English and Thai language articles from 1993 to 2018 available from six databases were used as data sources. Two independent reviewers assessed articles against the following eligibility criteria: experimental study, adult smokers 18 years of age, studies comparing the effectiveness of a smoking cessation intervention with no treatment or wait-list control, or usual care. Study quality was critically appraised by two reviewers using established criteria; Review Manager 5.1 was used for meta-analyses. Of the 77 eligible studies that were found, 15 had complete data for meta-analysis on PPA and/or wait-list control, or usual care. The meta-analyses indicated that smoking cessation counseling using quitline telephone counseling was the most effective strategy for smoking cessation on PPA when compared with no treatment or usual care. Conversely, other interventions resulted in nonsignificant differences between the experimental and control groups. In summary telephone counseling was found to be the most appropriate approach for facilitating smoking cessation in adult smokers in the primary healthcare setting. Further research is needed to compare the optimal course length, intensity, and long-term effectiveness for helping smokers quit in the primary healthcare setting.
Article Details
References
World Health Organization, WHO global report on trends in prevalence of tobacco smoking 2015, Geneva: World Health Organization, 2015.
J. E. Anderson, et al., Treating tobacco use and dependence:an evidence-based clinical practice guideline for tobacco cessation, Chest 121(3) (2002) 932 – 941.
K. Faulkner, et al., Are nurses and auxiliary healthcare worker sequally effective in delivering smoking cessation support in primary care?, Nicotine & Tobacco Research 18(5) (2016) 1054 –1060.
E. S. Smit, H. de Vries, C. Hoving, The PAS study: A randomized controlled trial evaluating the effectiveness of a web-based multiple tailored smoking cessation programme and tailored counselling by practice nurses, Contemporary Clinical Trials 31 (2010) 251 – 258.
L. S. Brose, A. McEwen, Neighbourhood deprivation and out-comes of stop smoking support–An observational study, Plos One 11(1) (2016) e0148194.
C. A. McGrath, et al., Smoking cessation in primary care: Implementation of a proactive telephone intervention, Journal of the American Association of Nurse Practitioners 26(5) (2014)248 – 254.
S. H. Zhu, et al., Telephone counseling for smoking cessation: Effects of single-session and multiple-session interventions, Journal of Consulting and Clinical Psychology 64(1)(1996) 202 – 211.
H. Brendryen, P. Kraft, Happy ending: a randomized controlled trial of a digital multi-media smoking cessation intervention,Addiction 103(3) (2008) 478 – 484.
J. F. Hollis, et al., Nurse-assisted counseling for smokers in primary care, Annals of Internal Medicine 118(7) (1993) 521 –525.
F. Tzelepis, et al., A randomised controlled trial of proactive telephone counselling on cold-called smokers’ cessation rates,Tobacco Control 20(1) (2011) 40 – 46.
J. F. Etter, Comparing computer-tailored, internet-based smoking cessation counseling reports with generic, untailored reports: a randomized trial, Journal of Health Communication 14(7) (2009) 646 – 657.
M. M. Clark, et al., Effectiveness of smoking cessation self-help materials in a lung cancer screening population, Lung Can-cer 44(1) (2004) 13 – 21.
S. L. Ridner, et al., Using motivational interviewing for smoking cessation in primary care, Southern Medical Journal 107(5)(2014) 314 – 319.
J. Percival, Smoking cessation: the role of the community nurse, Primary Health Care 10(3) (2000) 43 – 49.
B. Youdan, B. Queally, Nurses’ role in promoting and sup-porting smoking cessation, Nursing Times 101(10) (2005) 26.
S. A. Flocke, et al., A randomized trial to evaluate primary care clinician training to use the Teachable Moment Communication Process for smoking cessation counseling, Preventive Medicine 69 (2014) 267 – 273.
P. Aveyard, et al., A controlled trial of an expert system and self? help manual intervention based on the stages of change versus standard self?help materials in smoking cessation, Ad-diction 98(3) (2003) 345 – 354.
M. Unrod, et al., Randomized controlled trial of a computer-based, tailored intervention to increase smoking cessation counseling by primary care physicians, Journal of General In-ternal Medicine 22(4) (2007) 478 – 484.
P. Hongin, S. Preechawong, The effect of motivation program to quit smoking in orthopedic patients Thai Journal of Nursing 66(2) (2017) 11 – 17.
S. Haug, et al., Efficacy of a text message-based smoking ces-sation intervention for young people: a cluster randomized con-trolled trial, Journal of Medical Internet Research 15(8) (2013)e171.
M. Harter, et al., Evaluating a collaborative smoking cessation intervention in primary care (ENTER): study protocol fora cluster-randomized controlled trial, Trials 16 (2015) 447 –447.
H. Brendryen, F. Drozd, P. Kraft, A digital smoking cessation program delivered through internet and cell phone without nicotine replacement (happy ending): randomized controlled trial, Journal Of Medical Internet Research 10(5) (2008) e51.
N. E. Stanczyk, et al., Effectiveness of video-versus text-based computer-tailored smoking cessation interventions among smokers after one year, Preventive Medicine 82 (2016) 42 –50.
Bureau of Tobacco Control Department of Disease Control,The Second National Strategic Plan for Tobacco Control, 2015.
S. Benjakul, et al., Forecasting diseases & health hazard re-port: trend of tobacco consumption among Thai population,Bangkok: Nice earth design, 2014.
P. T. H. Julian, Cochrane handbook for systematic reviews of interventions, Hoboken, N.J.: Wiley, 2011.
D. Moher, et al., Preferred reporting items for systematic re-views and meta-analyses: the PRISMA statement, International Journal of Surgery 8(5) (2010) 336 – 341.
M. C. Fiore, et al., Treating tobacco use and dependence:2008 update US Public Health Service Clinical Practice Guide-line executive summary, Respiratory Care 53(9) (2008) 1217 –1222.
A. Mujika, et al., Motivational interviewing as a smoking cessation strategy with nurses: An exploratory randomised con-trolled trial, International Journal of Nursing Studies 51 (2014)1074 – 1082.
A. A. Jackson, et al., Beliefs and behavior of deceivers in a randomized, controlled trial of anti-smoking advice at a primary care clinic in Kelantan, Malaysia, 2004.
L. S. Skov-Ettrup, et al., The effectiveness of telephone counselling and internet- and text-message-based support for smoking cessation: results from a randomized controlled trial, Ad-diction 111(7) (2016) 1257 – 1266.
Bureau of Tobacco Control, Report of the first followup visit assessment of the national capacity to implement theMPOWER policy, Bangkok: WVOThaiprinting, 2011.
J. Usaha, D. Luemchan, T. Gunvihok, Evaluation on the National Strategic Plan for Tobacco Control 2012-2014, DiseaseControl Journal 42(2) (2015) 151 – 161.
World Health Organization, Developing and improving national toll-free tobacco quit line services: a World Health Organization manual, Geneva: World Health Organization, 2011.
World Health Organization, Developing and improving national toll-free tobacco quit-line services. Ginebra, Suiza:World Health Organization, 2011.
B. Bassett, New Zealand Country Report: Quit line Smoking Cessation Services, Asian Pacific Journal of Cancer Prevention17(S2) (2016) 25.
N. Nhung, et al., A national quit line service and its promotion in the mass media: modelling the health gain, health equity andcostutility. Tobacco Control 27(4) (2018) 434.