Knowledge and Practice on Tuberculosis Infection Control among Health care workers in Nay Pyi Taw, Myanmar
Main Article Content
Abstract
Introduction: Poor knowledge and inadequate practice on TB infection control (TBIC) can increase the risk of TB transmission among those directly responsible for TB, TB health care workers (TB HCWs), and general health care workers (General HCWs). The study aimed to compare the knowledge and practice on TBIC between these two groups and determine the predictors for the low level of knowledge and practice.
Methods: A cross-sectional study was conducted in Nay Pyi Taw, Myanmar, from September 2019 to January 2020. HCWs assigned for TB, multi-drug resistant TB (MDR-TB) care, diagnostic and prevention activities were included as TB HCWs, and those working at the general hospitals not directly responsible for TB patients were recruited as general HCWs. A total of 260 TB HCWs and 500 general HCWs were invited. Knowledge and practice on TB infection control among health care workers were assessed using the structured questionnaire. Participants were categorized as having low knowledge if their knowledge scores were below the mean score and likewise for practice.
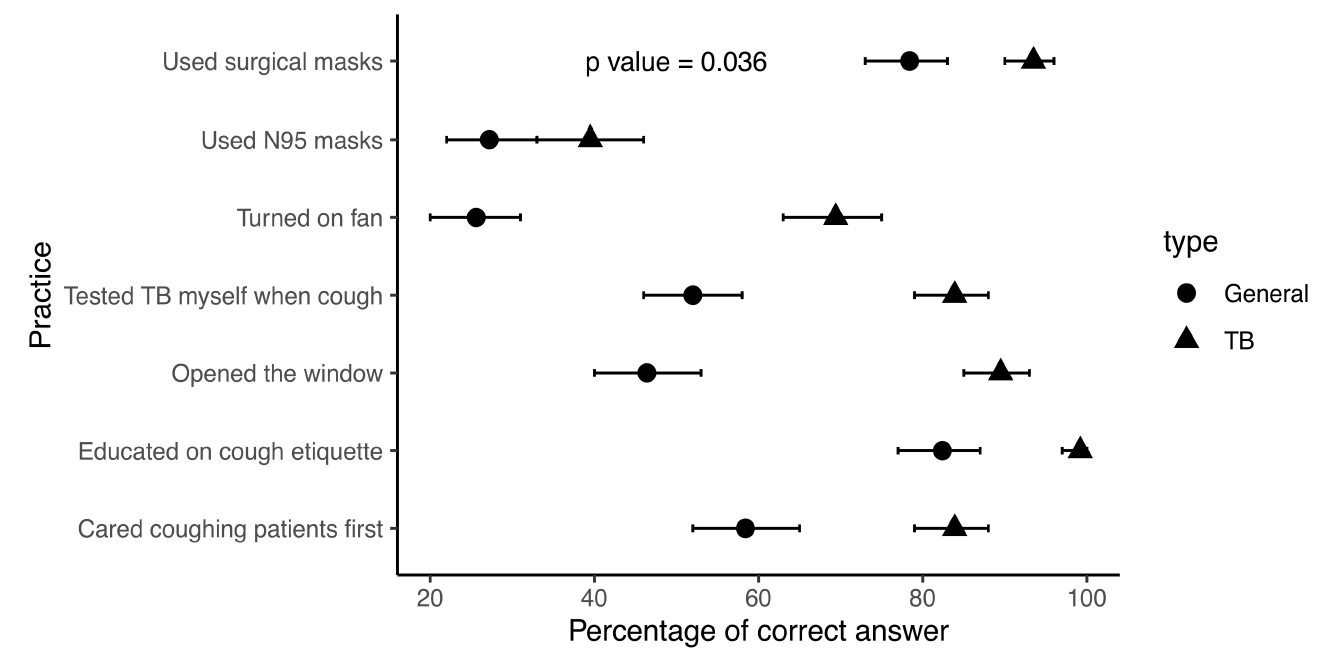
Results: Knowledge and practice scores were significantly higher among TB HCWs. With a maximum possible score of 10 for knowledge questions, the mean (SD) score of TB HCWs and general HCWs were 9.31 (0.987) and 7.35 (2.40), respectively, the p value of t-test 0.0095. With a maximum possible score of 7 for practice items, the mean (SD) score of TB HCWs and general HCWs were 4.718 (1.17) and 3.136 (1.441), respectively, the p value of t-test 0.036. Being ward staff and over 30 years old TB HCWs were the predictors of low knowledge. The predictors of poor practice were doctor, nurse, receptionist, ward staff, and those who had not been trained in TBIC.
Conclusion: More TBIC programme should be enhanced among health care workers, especially in risk groups, whose knowledge and practice were poor.
Article Details
References
T. Kompala, S. V. Shenoi, G. Friedland, Transmission of tuberculosis in resource-limited settings, Current HIV/AIDS Reports 10 (2013) 264 -- 72.
World Health Organization, Global Tuberculosis Report 2018, https://apps.who.int/iris/handle/10665/274453, 2018 (accessed 3 July 2018).
P. Birth, P. R. E. Behrman, A. S. Butler, et al., Tuberculosis in workplace, https://www.ncbi.nlm.nih.gov/books/NBK222453 (accessed 2001)
J. Du, Y. Pang, Y. Ma, et al., Prevalence of tuberculosis among health care workers in tuberculosis specialized hospitals in China, Journal of Occupational Health 59 (2017) 292 -- 295.
World Health Organization, Latent tuberculosis infection: updated and consolidated guidelines for programmatic management, https://www.who.int/tb/publications/2018/latent-tuberculosis-infection/en. (accessed 2018).
G. W. Comstock, V. T. Livesay, S. F. Woolpert, The prognosis of a positive tuberculin reaction in childhood and adolescence, American Journal of Epidemiology 99 (1974) 131 -- 138.
Stop TB Partnership, Key populations brief, http://www.stoptb.org/assets/documents/resources/publications/acsm/KPBrief_ HealthCareWorker_ENG_WEB.pdf. (accessed July 2017).
J. Jelip, G. G. Mathew, T. Yusin, et al., Risk factors of tuberculosis among health care workers in Sabah, Malaysia. Tuberculosis 84 (2004) 19 -- 23.
World Health Organization. Tuberculosis infection prevention and control 2019, https://apps.who.int/iris/bitstream/handle/10665/311259/9789241550512-eng.pdf. (accessed July 2019).
National Tuberculosis Program (Myanmar). Tuberculosis Infection Control Manual, https://www.challengetb.org/publications/tools/country/TB_Infection_Control_Manual_Myanmar_Eng.pdf. (accessed 2017).
H. J. Chapman, B. A. Veras-Estevez, J. L.Pomeranz, et al., Health care workers' recommendations for strengthening tuberculosis infection control in the Dominican Republic, Revista Panamericana de Salud Publica 42 (2019) 1 -- 9.
C. Q. Ngo, T. Manabe, G. Vu, et al., Difficulties in tuberculosis infection control in a general hospital of Vietnam: a knowledge, attitude, and practice survey and screening for latent tuberculosis infection among health professionals, BMC Infectious Diseases 19 (2019) 951.
O. H. Ajayi, A. Isiyaku, M. Balogun, et al., Knowledge and practice of TB infection control by health care workers at National Tuberculosis and Leprosy Training Centre, Zaria, North Western Nigeria, Acta Scientific Medical Sciences 3 (2019) 38 -- 46.
V. Pathak, Z. Harrington, C. C. Dobler, Attitudes towards preventive tuberculosis treatment among hospital staff, PeerJ 4 (2016) e1738.
M. Desta, T. Ayenew, N. Sitotaw, et al., Knowledge, practice and associated factors of infection prevention among healthcare workers in Debre Markos referral hospital, Northwest Ethiopia, BMC Health Services Research 18 (2018) 465.