Indoor Air Quality in Public Health Centers: A Case Study of Public Health Centers Located on Main and Secondary Roadsides, Bangkok 10.32526/ennrj/20/202200078
Main Article Content
Abstract
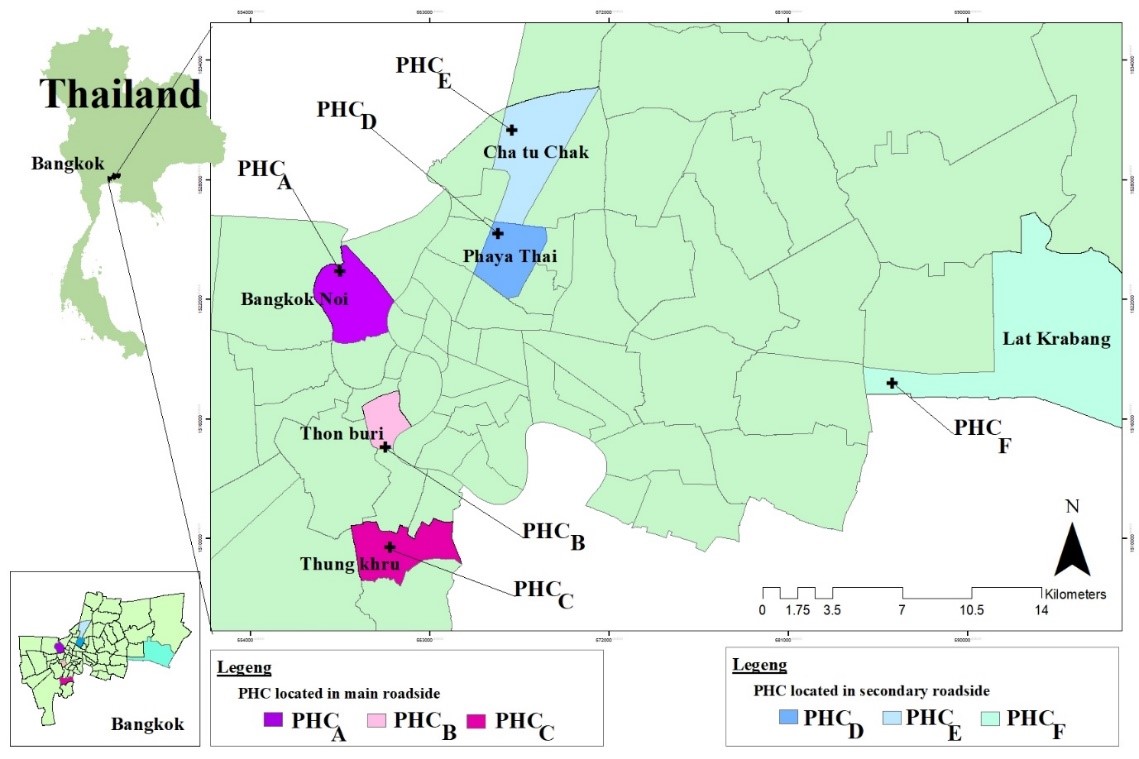
This cross-sectional study investigated the indoor air quality (IAQ) of public health centers (PHCs) and primary health care units in Bangkok to determine the impact of the different locations and ventilation systems concerning IAQ. Three indoor air pollutants: PM2.5, CO2, and CO were measured in three areas (medical record departments, outpatient departments and examination rooms) of six PHCs located in two different locations (main and secondary roadsides). The results showed that the average levels of PM2.5, CO2, and CO in the PHCs located on main roadsides were higher than those located on secondary roadsides. Among these parameters, only CO was found to significantly differ between those two locations indicating the result of vehicles and traffic sources regarding indoor CO level. Furthermore, all parameters were compared among the sampling areas with different ventilation systems; natural ventilation and air conditioner with and without ventilation fan. The amounts of all three pollutants significantly differed in each area with different ventilation systems. The average levels of PM2.5 and CO2 were the highest in areas with air conditioner without ventilation fan, while the level of CO was the highest in areas with natural ventilation. The ventilation was proved to be a key measure to improve IAQ. PHCs should consider ventilation efficacy to improve the IAQ by using ventilation fans in rooms using air conditioners. Finally, the average levels of all parameters were found below the recommended values in related standards, indicating safe IAQ for people working and receiving services in PHCs.
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Published articles are under the copyright of the Environment and Natural Resources Journal effective when the article is accepted for publication thus granting Environment and Natural Resources Journal all rights for the work so that both parties may be protected from the consequences of unauthorized use. Partially or totally publication of an article elsewhere is possible only after the consent from the editors.
References
American Conference of Governmental Industrial Hygienists (ACGIH). Threshold Limit Values for Chemical Substances and Physical Agents and Biological Exposure Indices. Cincinnati, Ohio: ACGIH; 2013.
Argunhan Z, Avci AS. Statistical evaluation of indoor air quality parameters in classrooms of a university. Advances in Meteorology 2018;2018;Article No. 4391579.
Babayiğit MA, Bakir B, TEKBAŞ ÖF, Oğur R, Kilic A, Ulus S. Indoor air quality in primary schools in Keçiören, Ankara. Turkish Journal of Medical Sciences 2014;44(1):137-44.
Brickus LS, Cardoso JN, Aquino Neto FR. Distributions of indoor and outdoor air pollutants in Rio de Janeiro, Brazil: Implications to indoor air quality in bayside offices. Environmental Science and Technology 1998;32(22):3485-90.
Bureau of Occupational and Environmental Diseases (BOED). Guide to measuring indoor air quality for Entrance and exit channels. 1st ed. Bangkok, Thailand: Aksorn Graphic and Design; 2018.
Chamseddine A, Alameddine I, Hatzopoulou M, El-Fadel M. Seasonal variation of air quality in hospitals with indoor-outdoor correlations. Building and Environment 2019; 148:689-700.
Chokwinyou P, Pensuk C, Paweenkitiporn W. Indoor air quality in hospitals and hotels, Thailand. Environmental Health Journal 2014;16:51-66.
Indoor Air Quality Management Group. Guidance Notes for the Management of Indoor Air Quality in Offices and Public Places. Hong Kong: Government of the Hong Kong Special Administrative Region; 2003.
Giulio MD, Grande R, Campli ED, Bartolomeo SD, Cellini L. Indoor air quality in university environments. Environmental Monitoring and Assessment 2010;170(1):509-17.
Hellgren UM, Palomaki E, Lahtinen M, Riuttala H, Reijula K. Complaints and symptoms among hospital staff in relation to indoor air and the condition and need for repairs in hospital buildings. Scandinavian Journal of Work Environment and Health 2008;34(4):58-63.
Karner A, Eisinger DS, Niemeier D. Near-roadway air quality: Synthesizing the findings from real-world data. Environmental Science and Technology 2010;44(14):5334-44.
Lee HJ, Lee KH, Kim DK. Evaluation and comparison of the indoor air quality in different areas of the hospital. Medicine (Baltimore) 2020;99(52):e23942.
Leung M, Chan AH. Control and management of hospital indoor air quality. Medical Science Monitor 2006;12(3):17-23.
Lomboy MFTC, Quirit LL, Molina VB, Dalmacion GV, Schwartz JD, Suh HH, et al. Characterization of particulate matter 2.5 in an urban tertiary care hospital in the Philippines. Building and Environment 2015;92:432-9.
Luksamijarulkul P, Somjai N, Nankongnap N, Pataitiemthong A, Kongtip P, Woskie S. Indoor air quality at different sites of a governmental hospital, Thailand. Nursing and Palliative Care 2019;4:1-5.
Mendes A, Pereira C, Mendes D, Aguiar L, Neves P, Silva S, et al. Indoor air quality and thermal comfort: Results of a pilot study in elderly care centers in Portugal. Journal of Toxicology and Environmental Health 2013;76(4-5):333-44.
Mullen NA, Bhangar S, Hering SV, Kreisberg NM, Nazaroff WW. Ultrafine particle concentrations and exposures in six elementary school classrooms in northern California. Indoor Air 2011;21(1):77-87.
National Institute for Occupational Safety and Health (NIOSH). Guidance for Indoor Air Quality Investigations. Cincinnati, Ohio: NIOSH; 1987.
Nimra A, Ali Z, Nasir ZA, Tyrrel S, Safdar S. Characterization of indoor air quality in relation to ventilation practices in hospitals of Lahore, Pakistan. Sains Malaysiana 2021; 50(6):1609-20.
Office of Public Health System Development, Health Department, Bangkok Metropolitan Administration. Annual reports and key statistics 2019 Bangkok [Internet]. 2020 [cited 2021 Sep 11]. Available from: https://webportal.bangkok.go.th /health/Annual-reports-and-key-statistics.
Pollution Control Department (PCD), Ministry of Natural Resources and Environment. Booklet on Thailand State of Pollution 2018. 1st ed. Bangkok, Thailand: S. Mongkon Press Limited Partnership; 2019.
Sompornrattanaphan M, Thongngarm T, Tantilipikorn P, Kreetapirom P, Foo J. The contribution of outdoor fine particulate matter to indoor air quality in Bangkok Metropolitan Region, Thailand: Are indoor dwellers safe? Siriraj Medical Journal 2018;70(4):265-71.
Synnefa A, Polichronaki E, Papagiannopoulou E, Santamouris M, Mihalakakou G, Doukas P, et al. An experimental investigation of the indoor air quality in fifteen school buildings in Athens, Greece. International Journal of Ventilation 2003;2(3):185-201.
Tang H, Ding J, Lin Z. On-site measurement of indoor environment quality in a Chinese healthcare facility with a semi-closed hospital street. Building and Environment 2020;173:Article No. 106637.
World Health Organization (WHO). WHO Global Air Quality Guidelines: Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide. Geneva, Switzerland: WHO; 2021.
Zhou Q, Lyu Z, Qian H, Song J, Möbs VC. Field-measurement of CO2 level in general hospital wards in Nanjing. Procedia Engineering 2015;121:52-8.
Zuraimi MS, Tham KW, Chew FT, Ooi PL. The effect of ventilation strategies of child care centers on indoor air quality and respiratory health of children in Singapore. Indoor Air 2007;17(4):317-27.